This is not a distant possibility, but the stark reality behind much of the "AI" and offshore digital labour fuelling dentistry today.
We were asked this question recently. At first glance, it appeared cynical. However, when we traced the evidence from AI supply chains to dental outsourcing, from regulatory duties to insurer audits, we discovered the concern is genuine. The market warrants a clear, evidence‑based approach discussion.
The Risk Everyone Overlooks
We support the sector's efforts to reduce energy use, promote recycling, and utilise sustainable materials. However, an equally important risk is being ignored: the human element in "digital" dentistry. Much of what is marketed as automation still relies on people, often located outside the UK, performing design and data tasks under standards that may not align with our own. This article calls for aligning clinical quality, regulatory accountability, and labour ethics throughout the entire supply chain so that the device in a patient's mouth reflects the values we stand for chairside.
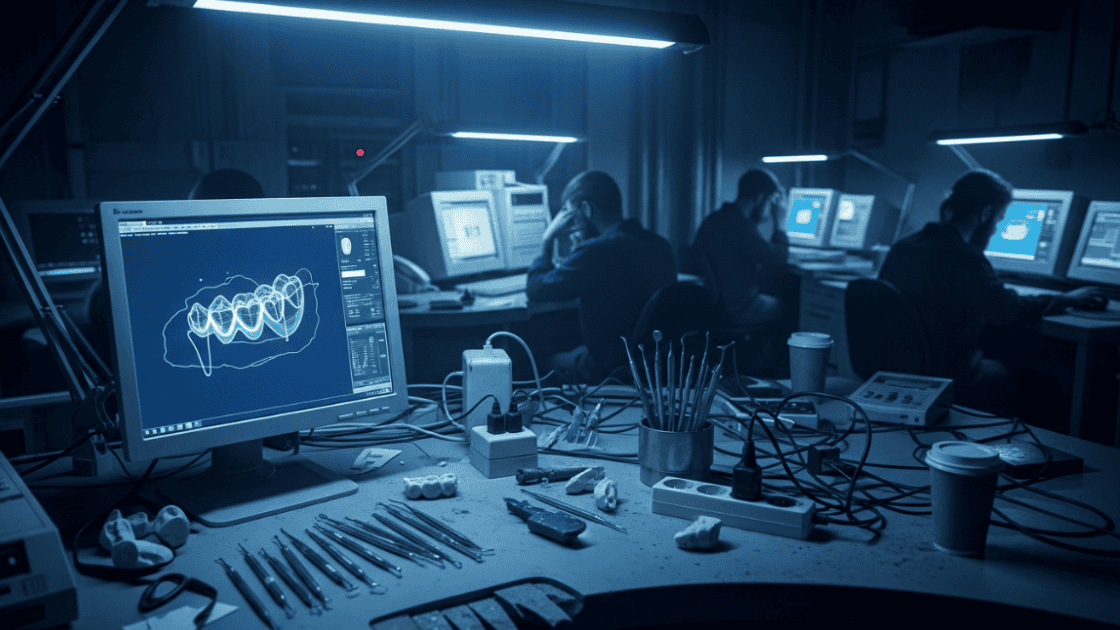
When "AI" Means Human Click Farms
We keep hearing about "AI‑driven dentistry." The glossy brochures suggest machines are doing the thinking. The reality is more prosaic and more uncomfortable. Behind many so-called AI platforms sit armies of people carrying out routine digital tasks, such as cleaning up scans, refining CAD files, and performing endless quality checks. In other industries, these workers have been documented as earning less than £2 an hour, often without proper safeguards. Dentistry is not immune to the same model.
Here is the clinical problem: invisible labour leads to invisible errors. A half-millimetre error in a rushed digital edit doesn't seem like much on a screen, but it becomes a chairside adjustment, an extra appointment.
If a workflow depends on anonymity and invisibility, ask what else is being hidden.
Who's Really Doing the Work?
Outsourcing isn't new to dentistry. What has changed is the speed and scale enabled by cloud platforms and on‑demand manufacturing. On the surface, they promise convenience: upload a file and receive a design or a finished part quickly. What's less obvious is who actually does the work, where it's done, and what standards apply. Too often, the answer is nobody really knows.
When price and turnaround are the only concerns, quality control often becomes an afterthought. Problems only surface once the case is in the chair. At that point, it's the UK clinician or lab left to fix the issues, not the offshore designer.
This isn't a plea to abandon digital partners. It's a call for basic transparency. If labs here are expected to meet strict regulations, then any supplier feeding into the same workflow should also meet those standards.
If a device is intended for a UK patient, it should be manufactured in accordance with standards you could defend before the GDC. Transparency is not just key; it is essential to uphold these standards.
Questions any "digital" vendor should be happy to answer
- Who, by legal entity and location, performs each step (design, CAM, manufacture)?
- What qualifications do those teams hold, and how are they supervised?
- Which materials and components are approved, and what is the substitution policy?
- What is your current remake or adjustment rate, and how is corrective action tracked?
- Where is patient data stored and processed, and under what legal regime?
- What labour standard do you apply (pay, hours, wellbeing), and when was it last audited?
Cheap Abroad Still Costs at Home
Energy efficiency and recycling targets are now common topics of discussion in the dental industry, and that's a positive development. But let's be honest, sustainability isn't complete if it overlooks the people doing the work.
If a design is created where staff are paid very low wages, without healthcare, protection, or recourse, can we truly say the supply chain is ethical? UK labs operate under strict employment laws. Minimum wage, health and safety, pensions, and support systems are built in.
Those standards come at a cost, but they are there to protect workers. However, if a UK professional unknowingly uses a product from an unethical supply chain, they may be unintentionally supporting labour exploitation, with serious legal and ethical consequences.
When design tasks are exported to low-cost settings, those protections don't transfer. What seems like a saving on the invoice can uncomfortably resemble an arbitrage of human rights.
However, the issue is on the radar. Major global partners and insurers now require suppliers to verify their policies and due diligence regarding modern slavery.
Modern slavery, which includes practices such as forced labour and human trafficking, is a serious concern and must be addressed to ensure ethical and regulatory compliance.
It's not just window dressing; it reflects a growing realisation that labour practices are part of clinical ethics. Patients expect us to uphold high standards throughout, not just in surgery.
The principle is simple. If we value UK labour rights, we shouldn't sideline them by pushing work offshore. The border doesn't alter the moral obligation.
Environmental metrics without labour standards are half a policy.
A genuinely ethical and sustainable dental industry should not compromise on either aspect, and it is our collective responsibility to ensure that both are given equal attention and importance.
The Illusion of Efficiency
On paper, outsourcing is an efficient solution. In reality, it often increases the workload for the very individuals it was supposed to ease.
Cases bounce back and forth: the offshore edit comes in, the UK lab reviews it, the surgeon examines it, modifications are requested, files are resent, and the cycle begins anew. By the time the appliance reaches the chair, multiple hands have handled it, and the expected time savings have disappeared.
This ongoing back-and-forth has tangible consequences. Technicians frequently spend more time reviewing and fixing than developing. Surgeons are drawn into design debates that should never involve them.
Cases drag on, patients wait longer, and reputations suffer when avoidable adjustments or remakes become the norm. Call it cynical if you like, but the pattern is familiar: the promise of low-cost efficiency upstream often results in hidden costs and frustration downstream.
The strain manifests as burnout in laboratories and frustration during surgeries. It also reveals a harsh truth: shifting work to lower-cost labour upstream doesn't eliminate the workload; it merely reallocates it, often onto the shoulders of skilled UK professionals who already carry the regulatory burden.
If efficiency is the goal, the better approach is to invest in quality at the source. A file done correctly the first time doesn't require three rounds of checks. That is where real productivity lives.
If You Can't Show the Paperwork, You Carry the Risk
Outsourcing the work does not transfer the responsibility. Under UK law, the prescribing dentist and the lab remain accountable for the appliance once it is placed in a patient's mouth.
That means if a crown fails, if a bridge doesn't meet medical device standards, or if paperwork is missing, the GDC or MHRA won't be looking for an offshore technician; instead, they'll be focusing on us.
Every device requires a signed statement, a named manufacturer, a materials list, and proof of compliance with the relevant regulations. If you don't have that, you're liable. These obligations don't disappear when files are sent abroad. They firmly rest on the shoulders of the clinician and the lab that supplied the device to the patient.
The message for practices and labs is clear: if you don't have this paperwork, you carry the risk.
Documentation every custom‑made device should have before fitting
- Statement of manufacture (signed and dated).
- Identification of the manufacturer or UK Responsible Person.
- Description of the device, including materials used.
- Confirmation that the device is intended exclusively for one patient, named on the form.
- Declaration of conformity with Medical Device Regulations.
- Record of any special characteristics requested by the prescriber.
The True Cost of a "Cheap" Crown
Cheap rarely means cheerful in dentistry. Think of it as the overall cost of ownership. A single remake doesn't just consume another block of zirconia; it also requires an extra hour of the surgeon's time, an additional appointment slot, more sterilisation, extra staff time for logistics, and often a difficult conversation with the patient. By the time all this is added up, the so-called savings have been wiped out.
Here's an example. Consider a practice that saves £40 per case by opting for a cheaper design service. If even 1 in 20 cases requires a remake, that single failure offsets the profit made on the previous 19. Add the opportunity cost of an hour of lost chair time, often valued at £500 or more, and the figures clearly turn negative. The cheapest option quickly becomes the most unprofitable.
And behind the economics lies a structural reality in which large manufacturers often profit most from the steady sales of components and implants. Meanwhile, the downstream burden of rework and delays falls on local labs and surgeries. The more the design quality is diluted, the greater the imbalance grows.
The lesson is clear: cost per unit is not the right metric. What truly matters is predictability, first‑time fit, and minimal rework. That's where genuine value exists for the patient, the surgeon, and the lab.
Pushing for Standards Isn't Anti-Innovation
Anyone familiar with us knows that we are a pro-industry laboratory. We have established our reputation by helping practices adopt new tools and techniques.
But they also know we're unafraid to highlight anything that jeopardises patient safety or undermines the profession itself. That's the spirit behind raising these concerns.
We are not anti-innovation; we live and breathe it. We've invested heavily in digital workflows and new materials, and we champion new tools every day. But innovation only counts if it delivers safe and reliable outcomes. Transparency and quality are what make new technology worth adopting.
Second, let me be clear, outsourcing itself is not the villain. The difference lies in how it's done. Some providers outsource openly, pay fair wages, and publish audit trails. That's responsible practice. The concern is that outsourcing can hide who is doing the work and under what conditions.
Third, price matters, but predictability and safety are more important. A single remake can eliminate the profit from twenty "cheap" cases.
Our stance is that higher standards protect patients, support clinicians, and safeguard the profession. That's how we ensure progress is sustainable.
What Every Supplier Should Guarantee
If, as a profession, we want to raise the standards, we need a clear, agreed-upon definition of what "good" looks like. Not in theory, but in practice, what every clinic and lab should expect from a digital supplier before they trust them with a patient's case.
Here's our perspective on the baseline:
- Know where it's made. Named production locations and legal entities, with proof of MHRA/MDR compliance.
- Respect for individuals. A written labour standard covering fair pay, reasonable hours, and mental health support where needed.
- Traceable materials. Clear documentation of materials and components used, and a policy on substitutions.
- Quality on record. Regular QC metrics, including remake rates, turnaround variance, and corrective actions, are shared openly.
- Data protection. A statement on where patient data is st