Dental implants have come a long way, restoring smiles, strength, and confidence. But one thing they’ve never restored is sensation. The subtle feeling of pressure when you chew. The feedback that guides your jaw on how hard to bite. That quiet connection between tooth and brain has been missing… until now.
A next-generation dental implant prototype is restoring something titanium could never do: the ability to feel. This breakthrough has the potential to significantly enhance the patient experience and reshape the future of dental care.
Here’s what this breakthrough means for your patients, your practice, and the laboratories that support both.
Dental implants have proven to deliver in terms of strength, aesthetics, and stability. However, they have consistently fallen short in one crucial aspect: sensation.
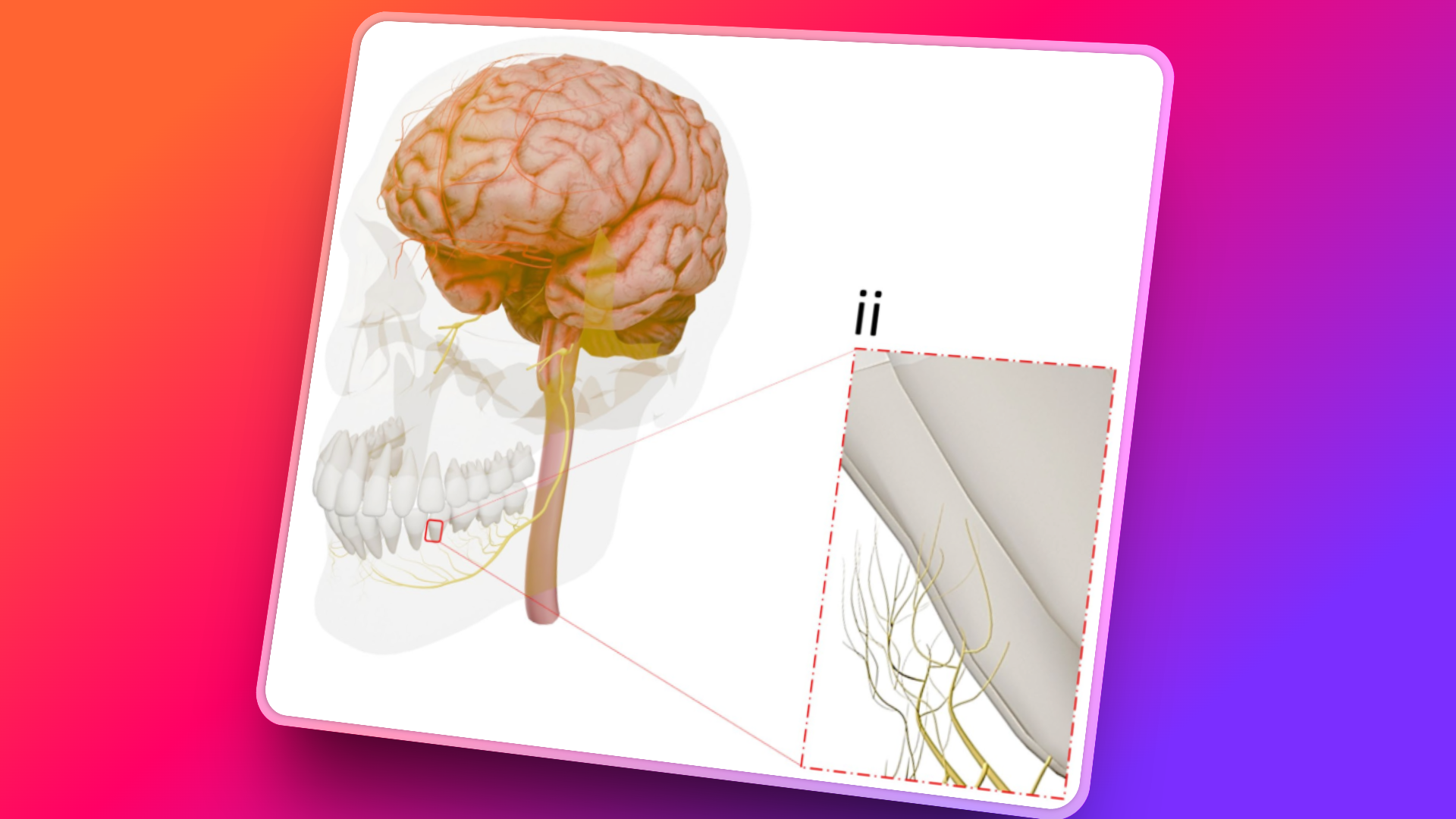
Without a periodontal ligament, conventional implants cannot send feedback to the brain. That missing feedback loop can impact fine motor control, chewing coordination, and even long-term wear patterns.
For most patients, it’s imperceptible—until it isn’t.
Now, a team of researchers at Tufts University is working to change that. They’ve prototyped a bioengineered, nerve-integrated implant that bypasses the bone fusion model entirely and instead reconnects with the nervous system.
This could signal the start of a new type of care: implants that restore function and sensation.
Let’s focus on what matters clinically:
Patients don’t focus on osseointegration. They want to eat confidently and chew without uncertainty. This implant takes us closer to that goal.
For dental surgeons, this is more than a product update; it’s a shift in protocol. The implant doesn’t integrate with bone—it interfaces with soft tissue and nerves. That alters everything from treatment planning to healing expectations.
Key shifts to expect:
This opens the way for dentists to provide a completely new value proposition: “Not just a replacement tooth, but one that feels like it’s part of you.”
This is where it becomes truly exciting.
Today, labs concentrate on mechanical fit, aesthetics, and strength. However, the next generation of restorative work will require something more profound: biological design thinking.
Your lab partner of the future won’t merely craft restorations; we’ll assist in engineering neural-compatible interfaces that integrate seamlessly with the body’s sensory systems.
The opportunity is clear:
“Smart implants are a clinical leap, not a technical tweak. For labs, this is a chance to step up, not step back.”
— Steve Campbell, Managing Director, Nexus Dental Lab
This technology is real, but it is still in its early phases. In preclinical trials, the Tufts team has successfully shown biocompatibility and initial nerve integration using rat models.
Within six weeks, the implants exhibited clear nerve-interface healing, with no signs of infection or inflammation. Notably, the implants were placed using a press-fit method, avoiding the need for traditional drilling altogether.
Each prototype was coated with biodegradable nanofibers, seeded with stem cells and the growth factor FGF-β, facilitating targeted regeneration of terminal nerve endings. Radiographic imaging revealed clean soft-tissue integration around the implant, with no evidence of bone contact, which differs from osseointegration and strongly indicates that the biological interface is functioning correctly.
This won’t replace traditional implants tomorrow. However, for certain patients—those requiring high-function posterior restorations, younger individuals, or cases where soft-tissue preservation is crucial—it may offer a superior physiological outcome.
And when it does arrive, the practices who lead will be the ones who have started thinking ahead.
Success won’t hinge on technology alone, but on the collective readiness across the dental space to work differently. This involves:
Labs, surgeons, and restorative teams alike will need to collaborate more closely than ever—not just to restore teeth, but to help patients reclaim a fuller sense of oral function.
We’re standing at the edge of something extraordinary. For the first time in implantology, we’re not just restoring structure; we’re on the verge of restoring feeling. This isn’t a marginal gain; it’s a fundamental shift in what dental treatment can offer: not just a tooth that fits, but a tooth that feels like it belongs. One that speaks to the brain, responds to the body, and behaves more like the one it replaced.
For clinicians, this opens a new frontier in treatment quality. For patients, it brings dentistry closer to biology than it has ever been. And for everyone in the dental profession—labs, surgeons, and technologists—it’s a moment to reconsider what’s possible… and to rise to the challenge.
The future of implants won’t just be smarter. It will feel more human because it is.
Das, S., Ghosh, S., Tu, Q., Zhu, Z.X., & Chen, J.J. (2025). Surgical considerations towards inducing proprioceptive feedback in dental implants. Scientific Reports, 15(15208). https://doi.org/10.1038/s41598-025-99923-8